ENSURE YOUR STUDENTS RECEIVE CLINICAL EXPERIENCE DURING THE PANDEMIC
16 TIPS FROM EXPERIENCED EDUCATORS FOR IMPLEMENTING YOUR OWN ACADEMIC-PRACTICE PARTNERSHIPS
Nursing leaders in Iowa and Idaho didn't wait long after a public policy was released by the nursing profession’s leading organizations last March.1
The brief recommended an increase in academic-practice partnerships between healthcare facilities and prelicensure nursing programs during the COVID-19 crisis. The purpose was to address both the growing burdens on nurses and the lack of available clinical sites for current RN students.
ATI researched the issue and talked to individuals who’ve been leading efforts in getting students back on the floor. Here, we've pulled together their top tips so that you can follow their lead and keep your students progressing toward graduation.
Discover how the Iowa and Idaho nursing leaders made their academic-practice partnerships a success.
(Watch NCSBN’s video interview with several of the nurse leaders who led the cause in their states.)
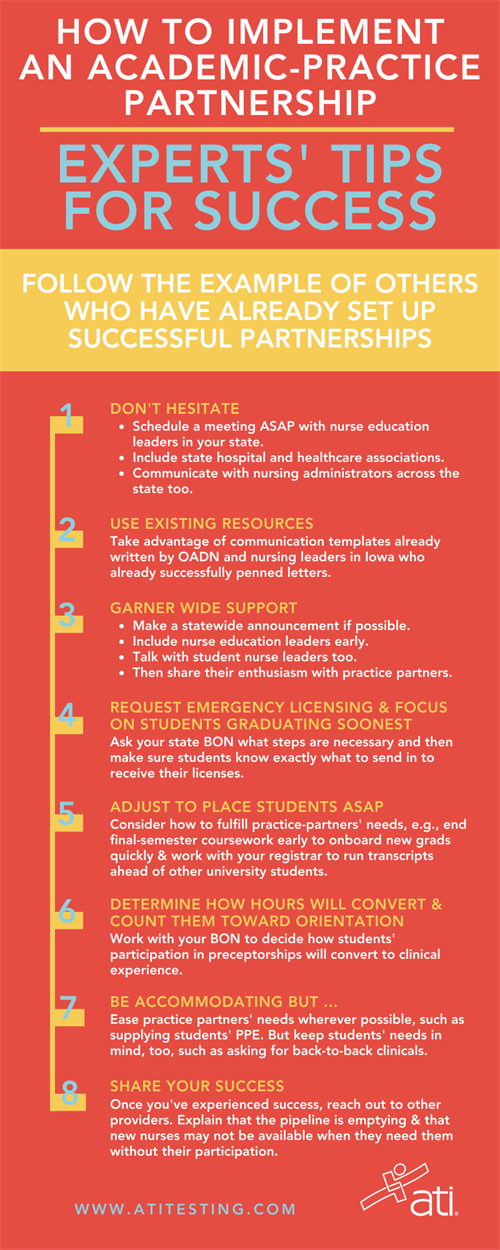
DOWNLOAD THE INFOGRAPHIC AS A HANDY REFERENCE
1) DON’T HESITATE.
As soon as you know the doors of nursing clinicals have closed — or you fear they might — act quickly. Schedule a meeting with all your state’s nurse education leaders, as well as state hospital and healthcare associations to begin discussing the situation. Ask them to share the information with their affiliates. Personally communicate with nursing administrators statewide.2) TWEAK EXISTING COMMUNICATIONS TO RECRUIT PARTICIPANTS.
Don’t waste time trying to write your own letter. Take advantage of a letter developed by Iowa nursing leaders and tweak it to work for your state's situation. Or use the customizable template created by the Organization for Associate Degree Nursing's COVID-19 Task Force. Send it to all nursing-related organizations and institutions in the state. Whenever an organization endorses the plan, ask them for permission to include their logo and signatory on an updated version to strengthen the letter’s impact and help sway others on the fence.3) MAKE A STATEWIDE ANNOUNCEMENT.
If possible, introduce the plan to develop practice-academic partnerships at some type of statewide conference or meeting. Conversing with a wider group allows for a diverse discussion around the model. But, in the current situation, take whatever steps you can to get the word out.4) GARNER AS MUCH SUPPORT AS POSSIBLE.
Include nurse education leaders in your conversations; get them involved early. Don’t forget about talking with student nurse leaders. Cultivate student ambassadors so they’ll share the idea of your partnership with their peers. Then communicate faculties’ and students’ commitment and excitement when you talk to practice partners.5) REQUEST EMERGENCY LICENSING.
Ask your state board of nursing what specific steps are necessary for it to approve and implement emergency licenses for students. Once you have the details, ask faculty to communicate them to students so they can deliver materials as quickly as possible to the BON.6) MAKE ADJUSTMENTS TO PLACE STUDENTS ASAP.
First, ask practice partners what they need to get students placed. Then, consider those needs from an academic standpoint. For example, to help onboard new grads quickly, end final-semester coursework early. Even just a few days can give your registrar’s office the chance to run transcripts ahead of the rest of the university's students, eliminating 2-3 weeks of time.7) DETERMINE HOW WORK HOURS WILL CONVERT.
Work with your BON in deciding how students' work in their preceptorships will convert to clinical experience. In Idaho, for example, the conversion was 1:1 — 1 hour of preceptorship equaled 1 hour of nursing clinical.8) FOCUS ON STUDENTS GRADUATING THE SOONEST.
Ask hospital partners to commit to making sure these students fully complete their internship hours to move them toward graduation as quickly as possible.9) ARRANGE FOR PRECEPTING HOURS TO COUNT AS EARLY ORIENTATION.
Faculty at Kirkwood Community College (Cedar Rapids, Iowa) encouraged seniors to work with potential employers to get precepting hours finished as an early orientation.10) VERIFY STUDENTS’ ELIGIBILITY.
Ensure that students who wish to participate have exhibited a certain level of knowledge and competence. To aid the process, name a coordinator to serve as a liaison between the academic institution and the practice partners.11) REDUCE RATIOS.
Ask your BON to consider reducing the ratio of instructor-to-student. If it’s typically 1:8, for example, suggest ratios of 1:4 or 1:5. This step removes the density and exposure issues that can burden providers.12) BE ACCOMMODATING, BUT REQUEST ADJUSTMENTS AS NEEDED.
Work with your practice partners in whatever ways possible to ease their situations. You may need to commit to supplying PPE (cloth masks and face shields) for students, for example. You also may need to revise PPE training or require students to redo PPE certification. Whatever the provider needs, do your best to meet their requests. But also keep in mind students’ needs. One program asked its hospital partner to allow clinical units to host back-to-back clinicals (day clinical and evening clinical), a practice the provider partner had previously denied.13) COMMUNICATE FREQUENTLY WITH YOUR MAIN PRACTICE PARTNER AND BON.
Once a partnership is in place, set up weekly meetings between all participants, including H.R. staff at the hospital. Communicate details of the emergency license plan and ask the hospital to identify what actions new graduates can and cannot perform during their preceptorships. Then help the provider move new grads into position quickly to begin orientation as early as possible. (Eventually, you can adjust the schedule of weekly meetings to every other week and then monthly.) Keep your BON in the loop, too, with regular reports of outcomes. Promise to meet any conditions it requires.14) AVOID LONG-TERM CARE FACILITIES.
COVID-19 research has proven the vulnerability to the novel coronavirus of individuals living in long-term care (LTC) facilities. During the current situation, then, you may want to weigh the benefits versus the risks of having students work with LTC residents. Young adults, in particular, may participate in high-risk behaviors you can’t control. Students also may work in jobs, such as hospitals or restaurants, that increase their exposure to the virus.15) FRONTLOAD NURSING CLINICALS IN THE FALL. BACKLOAD THEM IN THE SPRING.
Consider what epidemiologists and others are forecasting for the course of the virus. You may want to frontload clinicals at the beginning of the fall semester in case surges cause providers to shut down clinicals in October or November — despite partnership agreements. Assuming the virus is still rampant at the beginning of the spring semester, plan for nursing clinicals taking place at the end of that semester, allowing for catch-up in the summer if necessary.16) SHARE YOUR SUCCESS.
Once you have seen success with your initial practice partners, reach out to providers who didn't participate. Explain which facilities have gotten involved and how those providers will benefit (E.g., with committed students in preceptorships now who they can easily hire upon graduation later). Emphasize that the pipeline is emptying, and new nurses may not be available when the need arises if they don’t plan ahead.1American Nurses Association (ANA), National League for Nursing (NLN), National Council for State Boards of Nursing (NCSBN), American Organization for Nursing Leadership (AONL), American Association of Colleges of Nursing (AACN), Organization for Associate Degree Nursing (OADN), Accreditation Commission for Education in Nursing (ACEN), and Commission on Collegiate Nursing Education (CCNE).
ATI would like to thank these nursing education experts for their expertise in the development of the advice and information in this article:
- Maryann Alexander, PhD, RN, FAAN, Chief Officer, Nursing Regulation, NCSBN
- Kathy Dolter, PhD, RN, Dean of Nursing, Kirkwood Community College (Cedar Rapids, Iowa)
- Donna Meyer, MSN, RN, ANEF, FAADN, FAAN, CEO, Organization for Associate Degree Nursing (OADN)
- Anita Nicholson, PhD, RN, Professor (Clinical), Associate Dean for Undergraduate Programs, University of Iowa (Iowa City)
- Sarah Phipps, MSHSA, BSN, RN, Associate Executive Director of the State of Idaho Board of Nursing
- Julie Zerwic, PhD, FAHA, FAAN, Kelting Dean and Professor, College of Nursing, University of Iowa (Iowa City).
| ATI is working with programs just like yours to help them through the current challenges. From tips for moving your classroom online to best practices for using ATI’s solutions for online learning, testing, virtual simulation, and clinical hour replacement, we’ve got answers. Stay up to date on upcoming webinars, as well as those available in the archive of ATI Academy. Contact us to get more details on how ATI can help. |






.png?sfvrsn=7b705e9_0&MaxWidth=120&MaxHeight=&ScaleUp=false&Quality=High&Method=ResizeFitToAreaArguments&Signature=CE3B17E83B94410767F50179F69CB9C57767054A)