Teaching the 6 Functions of Clinical Judgment
How Active Learning Can Help You Develop Clinical Judgment in Nursing Students
After years of being the dominant conversation and concern in nursing education, has the urgency about teaching clinical judgment faded? Leading up to the introduction of clinical judgment measurement on the NCLEX in April 2023, faculty rallied to understand the NCSBN Clinical Judgment Measurement Model (CJMM) and prepare students for this momentous shift in testing. But many evaluation cycles later, some educators are still finding their footing when it comes to effectively teaching these critical skills.
The challenge isn't lack of interest. It's implementation. Despite understanding that clinical judgment is essential for nursing practice and NCLEX success, many programs haven't fundamentally changed how they are structured to deliver this teaching.
Meredith Watkins, DNP, MSN, RN, associate professor at the Elizabeth T. MacNeil School of Nursing at Dominican University, described it this way: Faculty loads are heavy, program resources are limited, and taking on the big lift of transforming teaching methods can feel daunting.
These issues can be addressed — even in the sometimes slow-moving world of academia. The solutions lie in the innate creativity and passion of nurse educators and the integration of evidence-based resources that provide active learning experiences.
Research shows that active learning strategies help educators foster critical thinking and support the development of clinical judgment.1-3 By anchoring active learning with a robust multimodal active learning environment, academic programs help ensure the development of strong clinical judgment skills in graduating students.
The 6 Cognitive Functions of Clinical Judgment
A review of the 6 functions of clinical judgment provides an important foundation for how to use active learning approaches when teaching this essential skill set
The clinical judgment process involves 6 functions nurses progress through when interacting with each patient. This process is iterative — nurses can gather new information or recognize cues while assessing or treating a patient, causing them to return to a previous function and move through the process again, continuously re-evaluating.
- Function 1: Recognize cues (assessment). This involves filtering information from different sources, including signs, symptoms, health history, and environmental factors. Recognizing cues in nursing practice is the foundational skill that sets everything else in motion.
- Function 2: Analyze cues (analysis). Here, nurses link recognized cues to the patient’s clinical presentation, establishing probable needs, concerns and problems. This is where pattern recognition and clinical knowledge intersect.
- Function 3: Prioritize hypotheses (analysis). Nurses establish priorities of care based on health problems, considering environmental factors, risk assessment, urgency, signs and symptoms, diagnostic tests, and lab values. The analyze cues-prioritize hypothesis connection is crucial for effective clinical decision making.
- Function 4: Generate solutions (planning). This function involves identifying expected outcomes and related nursing interventions to ensure patient needs are met. Generating solutions requires both creativity and evidence-based practice knowledge.
- Function 5: Take actions (implementation). Nurses implement appropriate interventions based on nursing knowledge, priorities of care, and planned outcomes to promote, maintain or restore health.
- Function 6: Evaluate outcomes (evaluation). Finally, nurses evaluate the patient’s response to nursing interventions and reach a judgment about the extent to which outcomes have been met.
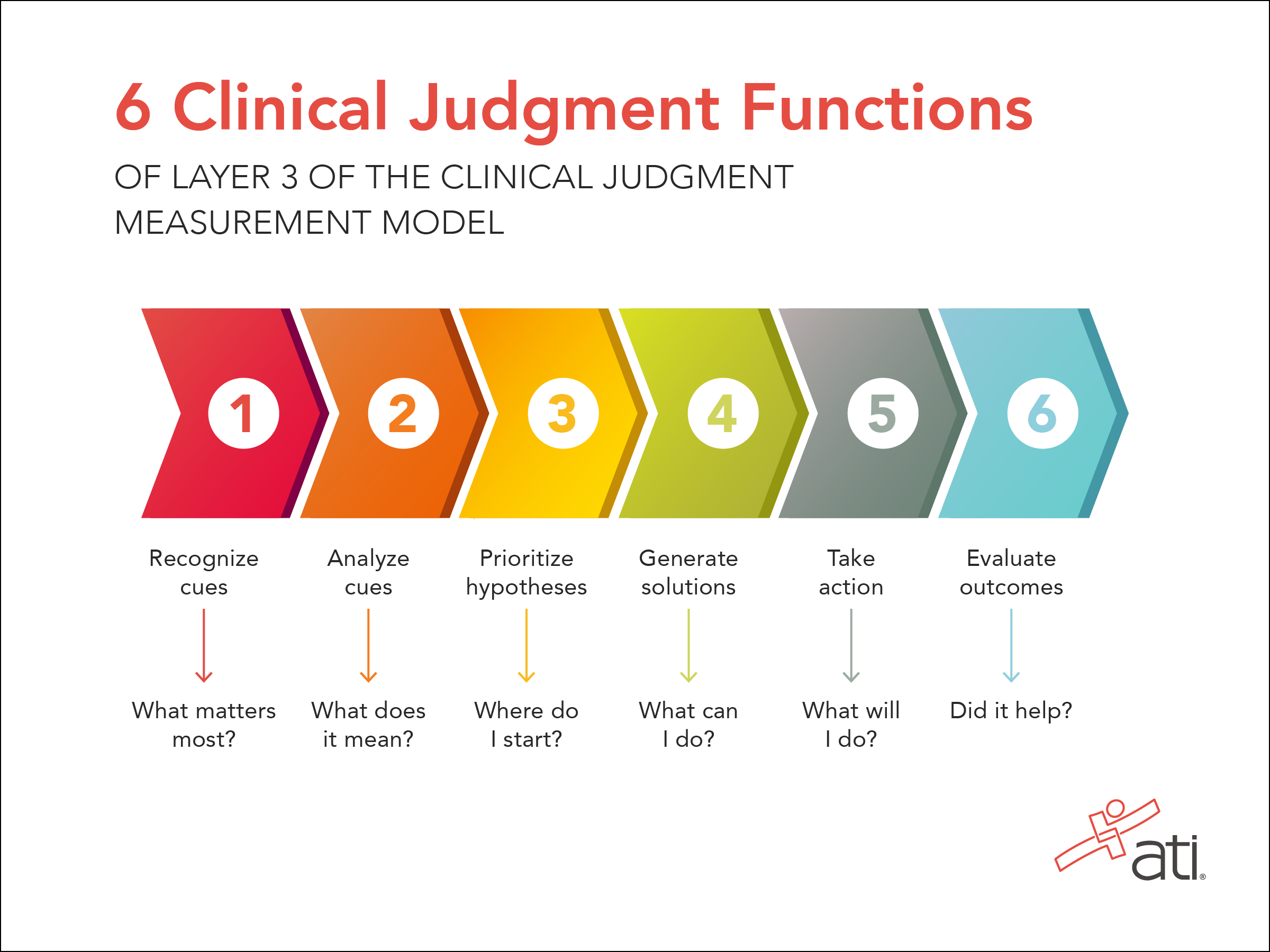
Understanding the relationship between the nursing process and clinical judgment — how the Clinical Judgment Measurement Model vs the nursing process work in tandem — helps students see that they're not learning something entirely new, but rather deepening and refining skills they're already developing.
The NCSBN Clinical Judgment Measurement Model
Before faculty can teach clinical judgment effectively, they need to understand what they’re teaching. The National Council of State Boards of Nursing (NCSBN) developed the CJMM to provide a framework for measuring clinical judgment and decision making on the NCLEX.4 (The visual representation of the CJMM is copyrighted by NCSBN and can be downloaded for nonprofit educational use here.)
The CJMM identifies the cognitive functions a nurse employs during decision-making, providing a systematic approach to what might otherwise feel like an enigma. It recognizes that a nursing process underlies the CJMM — but it is not one specific nursing process model. The NCSBN explicitly states that the clinical judgment model is not designed to replace any of the variety of nursing process models used across educational and clinical settings. No matter what model faculty use to teach the nursing process, good instruction will provide a solid foundation for students.
What Are the Challenges in Teaching Clinical Judgment?
In their 2024 study of barriers and facilitators to teaching clinical judgment, Carolyn Kerns, EdD, RN, FNP, CNE, and Monika Wedgeworth, EdD, RN, CNE, identified program, student and faculty factors as challenges.3
- Program factors included limited time, large class sizes and inconsistent clinical experiences.
- Student factors included poor preparation for class, variable critical thinking skills, tendency to focus on procedure or judgment, and personal challenges.
- Faculty factors included lack of professional development, confusion between critical thinking and clinical judgment, resistance to new pedagogies, and insufficient pedagogical knowledge.
 To Dr. Watkins, these challenges are familiar. She has encountered them in her own classrooms and during her work to develop courses on clinical judgment at two institutions. In an interview, she identified 2 primary barriers to providing effective clinical judgment instruction: understanding it and finding time to learn how to teach it.
To Dr. Watkins, these challenges are familiar. She has encountered them in her own classrooms and during her work to develop courses on clinical judgment at two institutions. In an interview, she identified 2 primary barriers to providing effective clinical judgment instruction: understanding it and finding time to learn how to teach it.
"I think as nurses, clinical judgment becomes something we just do," Dr. Watkins said. "But we aren't aware that we're doing it. And so we have to be able to call out the steps that we do in our own practice in order to then teach them."
She recalled a pivotal realization she reached early in her nursing career. After successfully starting all IVs on the first attempt during a shift, she proudly told her trainer about it. The trainer, a 30-year veteran ER nurse, bluntly responded: “Meredith, I could teach a monkey to start an IV. I want to teach you to critically think.”
Even as a seasoned nurse assigned to teach a clinical judgment course, Dr. Watkins struggled with the concept. “I thought that with clinical judgment, you either have it, or you don't. What do you mean, teach it?”
She sought out mentors and deeper learning, and she gained understanding that the process requires breaking clinical judgment into teachable components. She also determined that traditional lecture-based methods aren't sufficient for developing the complex cognitive skills that are required.
Bringing Clinical Judgment to Life Through Active Learning
Now, Dr. Watkins’ approach to teaching clinical judgment centers on active learning strategies that create space for students to practice the clinical judgment process repeatedly. Her method is built on 5 key principles:
1. Establish psychological safety and create a warm, welcoming environment.
Students need to feel safe about participating, knowing they won't be embarrassed, shut down, or yelled at when they make mistakes or share uncertain thinking, Dr. Watkins said. This safety is foundational to engagement.
2. Actively engage students by creating a class they're excited to attend.
Making learning fun isn't frivolous — it's strategic. Dr. Watkins keeps a drawer full of active learning supplies: paddles (thumbs up/thumbs down, whiteboard paddles), stickers, stars, rubber stamps, and her current favorite, tiny resin turtles that students collect and trade when they participate.
“I know it sounds so silly, but bright colors and fun random things really help engage learners,” she said. “At the heart of active learning is engagement, right? So the first thing I've got to do is keep their attention.”
3. Flip the classroom and make students accountable.
To create space for active learning, Dr. Watkins often uses a flipped classroom model. Students complete study guides with videos covering need-to-know content before class: signs and symptoms, risk factors, treatments, nursing assessments, and considerations.
She then confines lectures to 10-15 minutes, using one slide in class for quick review before jumping into activities. "Keep it short, keep it straightforward, and then let the nuances come from the case studies," she advised.
As an example, for her class on mental health, Dr. Watkins has assigned modules in Engage® Mental Health as prework. She then has students work through interactive scenarios that require them to recognize and analyze cues. During class, she builds on this foundation with case studies that push students to prioritize hypotheses and generate solutions — essentially moving them through the entire clinical judgment cycle.
Engage Mental Health is part of the Engage Series, an interactive technology-based learning environment providing multimodal resources that are unique within nursing education. When nursing programs integrate this comprehensive learning environment, students learn and perform better across core curriculum areas, including clinical judgment.5,6
4. Make clinical judgment visible and intentional. Repeat, repeat, repeat.
Dr. Watkins keeps NCSBN's clinical judgment skills cards in her classroom for students to reference during case studies or practice quizzes. She also turned the ATI Guide for Clinical Judgment graphic (shown below) into a sticker and placed one on every student's notebook. Dr. Watkins added that one of her colleagues hangs posters of the 6 clinical judgment functions in her classroom — keeping the process front and center. 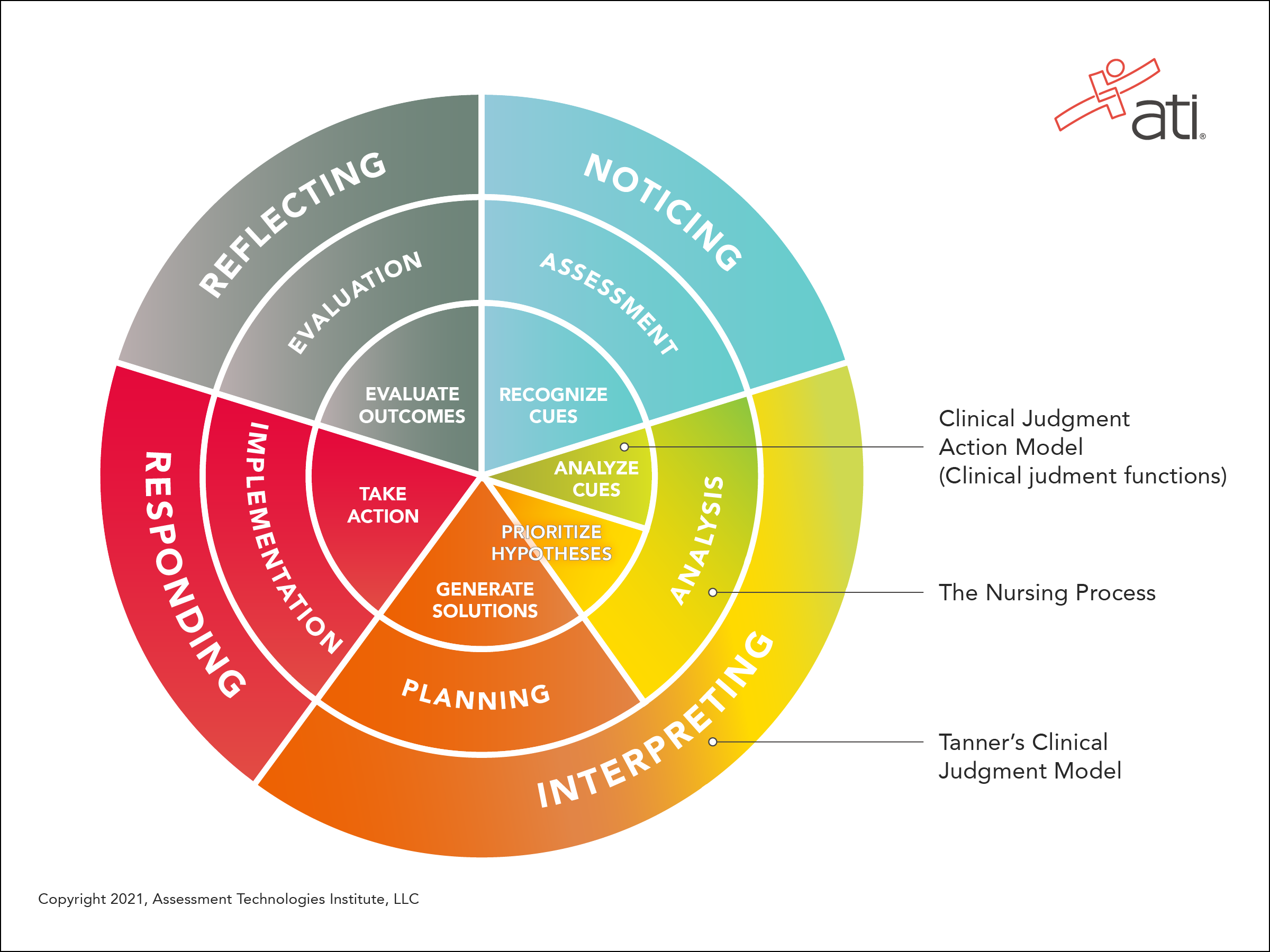
But visibility alone isn't enough. Educators need to repeat, repeat, repeat.
“Intentional scripting, over and over, is very important,” Dr. Watkins said. “It’s not just doing it, but asking 'what are we doing here?' We are analyzing cues, we are generating solutions. Using those words over and over is really important."
5. Mix up activities to maintain engagement.
Variety keeps students engaged and allows them to practice clinical judgment in different contexts. Each activity provides clinical judgment examples that students can internalize and apply. Dr. Watkins’ activities include:
- 6-part NCLEX-style case studies with cue cards
- Think-pair-share exercises
- Idea popcorn (rapid-fire sharing)
- Storytelling about clinical experiences
- Matching games (vocabulary terms with definitions)
- Competitive team activities.
Active Learning Is Proven to Build Clinical Judgment in Nursing Students
Dr. Watkins became a full-time educator in 2020, after 8 years as a clinical instructor. Her passion for teaching is evident — and so is her drive to contribute to scholarship and faculty development. As she saw students’ minds click as a result of active learning, she sought to determine if these techniques could be connected directly with student understanding of clinical judgment.
The answer? Yes. Using a quasi-experimental design, she evaluated the impact of active learning on clinical judgment. The resulting study, published in Teaching and Learning in Nursing in 2025,1 documented that active learning was more effective than passive learning in developing clinical judgment — specifically the function of interpreting/analyzing. She documented a 10-point difference between students in the active learning and the passive learning groups. Read more about the findings in this article about active learning on the ATI Educator Blog.
The Path Forward: Amplify Clinical Judgment Teaching With Proven Resources
As new graduates face higher acuity patients and fewer resources, clinical judgment skills are more critical than ever. The good news? You don't need to overhaul your entire program overnight.
Start by understanding the 6 functions of clinical judgment, breaking the process into teachable components, and incorporating active learning strategies where students practice repeatedly.
Even small changes — such as flipped content delivery, case study analysis, and intentional scripting of clinical judgment language — can yield significant results.
The Engage Series amplifies these efforts by providing a unified multimodal environment where students learn, practice, assess, and remediate clinical judgment skills. With ready-to-use lesson plans, interactive case studies, and analytics aligned to NCLEX content, Engage gives you the scaffolding to implement active learning without adding to your already heavy workload.
When students are more engaged, learning becomes more meaningful and effective. And when you have the right tools and strategies in place, clinical judgment becomes less daunting and more rewarding — for both you and your students.
References
- Watkins M, Fruin BW, Brett A. Using Active Learning to Develop Clinical Judgment in Nursing Students. Teaching and Learning in Nursing. 2025;20(4):e1170-e1175. https://doi.org/10.1016/j.teln.2025.06.005
- Wankier J, Beynon C. Enhancing Clinical Judgment in Undergraduate Clinical Education. Teaching and Learning in Nursing. 2025;20:32-36. https://doi.org/10.1016/j.teln.2024.08.019
- Kerns C, Wedgeworth M. Barriers and Facilitators Experienced by Undergraduate Nursing Faculty Teaching Clinical Judgment: A Qualitative Study. SAGE Open Nursing. 2024;10:1-11. DOI: 10.1177/23779608241274728
- NCSBN. Clinical Judgment Measurement Model. A Framework to Measure Clinical Judgment & Decision Making. https://www.nclex.com/clinical-judgment-measurement-model.page
- ATI Nursing Education, 2025. Data collected from proctored ATI RN and PN student assessment results (N=52,447), fall 2024 semester.
- CSAT data, 2025. In a national survey of nurse educators (N=474), 97% said ATI has a positive influence on student clinical judgment.

