7 EXPERTS REVEAL BEST PRACTICES FOR CLINICAL PREP
THE CONSEQUENCES WHEN STUDENTS LACK CONFIDENCE IN CLINICAL
 You don’t need a stack of research articles to know nursing students typically lack confidence when they enter the clinical setting. You can likely speak from personal experience about the fear and uncertainty students have described after the first time they interacted directly with clients.
You don’t need a stack of research articles to know nursing students typically lack confidence when they enter the clinical setting. You can likely speak from personal experience about the fear and uncertainty students have described after the first time they interacted directly with clients.Research, however, does support that gut feeling of nervousness you have on behalf of your students.
In June, an article in the "Journal of Professional Nursing" noted:
“Due to the demanding nature of critical-care settings, students are prone to experience stress and lack of confidence, which hinders their learning and affects patient care.”1
An even more recent article, in the July issue of "Nurse Education Today," noted:
“Many students have anxiety about clinical rotations.”2
But what specifically is the result of students who lack confidence when they enter the clinical setting?
What can you do to help?
And how can you support students whose negative clinical experience exacerbates their lack of confidence?
We asked 7 seasoned, expert nurse educators for some advice.
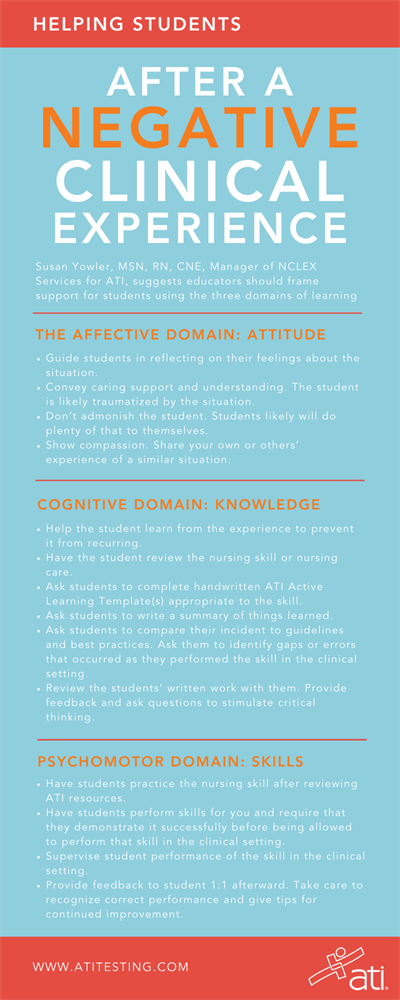
DOWNLOAD THE INFOGRAPHIC AT RIGH AS A HANDY REFERENCE
Q: WHAT HAPPENS DURING CLINICALS TO A STUDENT WHO LACKS CONFIDENCE?
 Larissa Bair, MSN, RN, CEN, has seen insecure new nurses and students flounder in her career as a preceptor in the E.R., as a faculty member for several nursing programs, and in her current role as an NCLEX Services Manager for ATI.
Larissa Bair, MSN, RN, CEN, has seen insecure new nurses and students flounder in her career as a preceptor in the E.R., as a faculty member for several nursing programs, and in her current role as an NCLEX Services Manager for ATI.
“When a new nurse lacks confidence in clinicals, they are unable to safely advocate for patients,” Bair says. “A lack of confidence can cloud judgment or make a nurse second-guess their clinical decision-making. Being confident in clinicals can lead to safer outcomes for patients,” she explains.
 Dianna Johnston, DNP, RN, NE-BC, CNE, has seen the same outcomes with students. A decorated wartime veteran who served in the U.S. Air Force and has received numerous teaching awards, Dr. Johnston currently works as a Nursing Education Consultant for ATI. She says that students who lack confidence in the clinical setting can present in myriad ways.
Dianna Johnston, DNP, RN, NE-BC, CNE, has seen the same outcomes with students. A decorated wartime veteran who served in the U.S. Air Force and has received numerous teaching awards, Dr. Johnston currently works as a Nursing Education Consultant for ATI. She says that students who lack confidence in the clinical setting can present in myriad ways.
“They will find ways to ‘live’ in the areas of comfort,” she explains. “For instance, if they are a CNA, they will focus on those tasks they know well. Although the facilities appreciate that help, it detracts from the students’ ability to think and act like a nurse.”
Similarly, students may ask their instructor or assigned nurse to “let them watch” rather than performing the nursing skill. “Others,” she adds, “may find places to hide.”
On the more ominous side, she says, students may present with a false sense of security. That facade can put a patient at risk.
“These students require much more supervision,” she explains, “and that takes the instructor away from the remaining student group.”
Q: HOW CAN AN EDUCATOR AID A STUDENT IN UNDERSTANDING THE IMPORTANCE OF PRACTICE BEFORE CLINICALS TO BUILD CONFIDENCE?
 “Students don’t know what they don’t know,” says Karen Taylor, DNP, RN, BSN, MSN. “In other words, they’ve never been on the floor, trying to do one skill on one patient, while there are 20 other skills and patients that need to be addressed, while charting on the last 20 things you did, while a provider is asking you questions, and the call light is going off … and on and on.”
“Students don’t know what they don’t know,” says Karen Taylor, DNP, RN, BSN, MSN. “In other words, they’ve never been on the floor, trying to do one skill on one patient, while there are 20 other skills and patients that need to be addressed, while charting on the last 20 things you did, while a provider is asking you questions, and the call light is going off … and on and on.”
Dr. Taylor’s experience as a labor and delivery nurse, travel nurse, staff nurse, and educator eventually led to her position as an Integration Specialist Nurse Educator at ATI. She’s seen how anxious students can get while learning the most basic nursing skills — which, in actuality, are extremely complex. And that complexity is intensified when students suddenly must perform multiple skills simultaneously.
She recommends advising apprehensive students to practice skills as much as possible before stepping foot in a clinical setting.
“By practicing in a ‘safe’ environment, like virtual simulations,” she says, “they can focus on feeling comfortable with individual skills or concepts without the fear of hurting the patient or the distractions of multi-tasking.”
Building that confidence gives the student a better chance of success in multi-tasking, communicating with providers and clients, and performing other, more complex tasks, she explains.
“Clinicals are filled with pressure, and students become overwhelmed, because they are so task-oriented,” she adds. “Practicing prior to the real thing is key to a successful experience.”
Q: HOW CAN AN EDUCATOR BUILD THE CONFIDENCE OF A STUDENT WHO HAD A NEGATIVE EXPERIENCE IN CLINICALS?
Educators often assign reflection homework to help students better understand their learning, and that assignment is especially useful for students in clinicals — especially students who leave the clinical setting more harried than when they went in.
Kendra Lindloff, MSN, RN, CNE, knows from her own clinical experience how effective reflection can be. Having worked in peri-operative care, surgery, staff education, pediatrics, and medical-surgical nursing, she has since applied her expertise to working as an Integration Specialist Nurse Educator for ATI.
“To regain confidence in clinical performance,” Lindloff explains, “it is important for students to reflect upon their experience — whether good or bad — and look for the learning opportunities.”
She asks students to reflect on what went well, what could have been done differently, their thought processes, and emotions.
“After reviewing, students should ask themselves how they will incorporate new clinical habits or behaviors into their practice,” she advises.
.png?sfvrsn=58a405e9_0&MaxWidth=200&MaxHeight=&ScaleUp=false&Quality=High&Method=ResizeFitToAreaArguments&Signature=E415B4EF1EE399AF36939FB8585AFDAA5EFEF2E0) Reflection is part of the same advice offered by Susan Yowler, MSN, RN, CNE.
Reflection is part of the same advice offered by Susan Yowler, MSN, RN, CNE.
An RN since 1984, Yowler spent more than 20 years in practice as a maternal newborn nurse. She worked with thousands of student nurses during those years and during her tenure as an instructor in several nursing programs.
“I think it’s crucial for the educator to have a conversation with the student to debrief,” she adds.
“Frame the support to the student using the three domains of learning,” she suggests.
Yowler provides tips for each domain:
1. Affective domain (Attitude)
- Guide students in reflecting on their feelings about the situation.
- Convey caring support and understanding to the student. “They’re likely traumatized by the situation,” she says.
- Don’t admonish the student. “The student likely will do plenty of that to themselves,” she points out.
- Show compassion. “Share your own or others’ experience of a similar situation,” she advises.
2. Cognitive domain (Knowledge)
- Help the student learn from the experience to prevent it from recurring.
- Have the student review the nursing skill or nursing care. (She recommends ATI Skills Modules, Video Case Studies 2.0, or Real Life Clinical Reasoning Scenarios.)
- Ask students to complete handwritten ATI Active Learning Template(s) appropriate to the skill.
- Ask students to write a summary of things learned from viewing the ATI resources.
- Ask students to compare their incident to guidelines and best practices. “Ask them to identify gaps or errors that occurred as they performed the skill in the clinical setting,” she suggests.
- Review the students’ written work with them. “Provide feedback and ask questions to stimulate critical thinking,” she advises.
3. Psychomotor domain (Skills)
- Have students practice the nursing skill after reviewing ATI resources.
- Have students perform skills for you and require that they demonstrate it successfully before being allowed to perform that skill in the clinical setting.
- Supervise student performance of the skill in the clinical setting.
- Provide feedback to student 1:1 afterward. “Take care to recognize correct performance and give tips for continued improvement,” she adds.

Another tip: Ask students who have negative clinical experiences to describe what their expectations were for clinical, says Debbie Wallace, PhDc, RN, MSN.
Dr. Wallace’s decades of nursing experience range from working as a school nurse and RN, as well as instructor for multiple nursing programs.
“I would want to know more about that bad experience,” she says. “Was it with an instructor or staff? Was it because the student did not meet the objectives?”
Faculty have a responsibility to provide remediation for students, she explains, so they can master a skill or knowledge.
Currently working as an Integration Specialist Nurse Educator at ATI, Dr. Wallace says that, on the first day of clinical, she asks students, “Who wants to be the best nurse ever?”
“They all raise their hands,” she says. “I continue to explain that I may provide feedback that is not flattering. I do that because I want them to become the best nurse ever! It is my role to help to facilitate their learning in the clinical experience. When providing feedback, I always ask the student first, ‘What do you think you did well/or what could you improve?’”
Often, she says, the student is more critical of their efforts than she is.
Even so, she says, “I will sandwich the feedback for the student and start by telling them what they did well, then how to improve, and then end with a positive.”
 Lindsey Blalock, MSN, APRN, WHNP-BC, has a similar outlook in questioning and supporting students. Blalock, who has been providing nursing care since 2005 as a women’s health nurse practitioner, also works as an Integration Specialist Nurse Educator at ATI.
Lindsey Blalock, MSN, APRN, WHNP-BC, has a similar outlook in questioning and supporting students. Blalock, who has been providing nursing care since 2005 as a women’s health nurse practitioner, also works as an Integration Specialist Nurse Educator at ATI.
She suggests considering some of the external factors that may have contributed to the student’s negative experience.
“We have to really look at all aspects of the clinical environment,” she says. For example, give some thought to:
- Did the student have a thorough orientation to the unit and tools used on the floor (computer/charting methods/vital sign machine/etc.)?
- What type of relationship does the student have with you, the educator, as well as the staff on the floor and with peers?
- How is the student doing in didactic and other clinical courses? Is that student struggling somewhere else, as well?
- Was the student immersed in a clinical situation that was appropriate (or handled appropriately) for all healthcare personnel that were involved?
- Did the student use logical and theoretical frameworks for decision-making?
“Once we have a better understanding of where the breakdown occurred, we — as educators — can then go back and direct the student for appropriate remediation,” Blalock explains.
She says you can build up students’ confidence by reminding them to be patient and kind to themselves during the learning experience. “Remind them to be open to feedback and to take remediation work seriously, so they can meet your clinical objectives in an appropriate manner and in a realistic time frame.
“Students often are fearful and, at times, unsuccessful in meeting clinical objectives,” Blalock adds. “But it’s important for them to realize that it takes time to acquire the knowledge needed to be successful in nursing school.”
RESEARCH SUPPORTS EDUCATORS’ ADVICE
 Research reinforces the outcomes of the advice offered by these educators. The "Nurse Education Today" article cited earlier, for example, concludes with:
Research reinforces the outcomes of the advice offered by these educators. The "Nurse Education Today" article cited earlier, for example, concludes with:
“Strategies that nurse educators can use prior to, during, and after the clinical experience to address student concerns about clinical experiences include the use of caring, competent clinical instructors, orientation to clinical sites, nursing simulation and lab days, self-reflection, peer-support, and debriefing.”2
Similarly, as suggested in the reference above, as well as by several educators interviewed here, nursing simulation can be an important part of building students’ confidence. The previously cited "Journal of Professional Nursing" states, “To enhance student preparedness for effective practice, high-fidelity simulations and course-based teaching have been demonstrated to be effective.”1
A January 2020 article in "Nurse Education in Practice" offered similar facts, stating, “Strong evidence exists that simulation improves clinical skills and raises confidence and decision-making for undergraduate nursing students.”3
Earlier research also reinforces recent studies about the impact of nursing simulation on student confidence, including one in January 2016’s edition of "Nurse Education Today," which stated, “Repeated simulation experiences can lead to an increase in student confidence and active learning.”4
NEW SIMULATION OPTIONS BUILD CLINICAL CONFIDENCE
 A new option for educators wanting to boost their students’ confidence is a nursing simulation offering from ATI: Video Case Studies 2.0. This solution has been created to offer an easier way for students to grasp difficult concepts. Live-actor video scenarios help students visualize what to expect in clinicals, ending with a prompt. Students exercise clinical judgment skills to form and articulate their own plan of care, then hear an expert response, which they consider as they complete a self-reflection.
A new option for educators wanting to boost their students’ confidence is a nursing simulation offering from ATI: Video Case Studies 2.0. This solution has been created to offer an easier way for students to grasp difficult concepts. Live-actor video scenarios help students visualize what to expect in clinicals, ending with a prompt. Students exercise clinical judgment skills to form and articulate their own plan of care, then hear an expert response, which they consider as they complete a self-reflection.
Nursing simulations like Video Case Studies 2.0 can ensure students are prepared for clinicals and boost their confidence by providing greater exposure to clinical situations and experience making clinical decisions.
1Nursing students’ preparedness and practice in critical care settings: A scoping review. (2020, June 12). ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S8755722320301307?via%3Dihub
2Self-efficacy and concerns of nursing students regarding clinical experiences. (2020, July 1). ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S0260691719313644
3Undergraduate nursing student perceptions of directed self-guidance in a learning laboratory: An educational strategy to enhance confidence and workplace readiness. (2020, January 1). ScienceDirect. https://www.sciencedirect.com/science/article/pii/S1471595318302518
4Can nursing students’ confidence levels increase with repeated simulation activities? (2016, January 1). ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S026069171500461X

