HOW POOR COMMUNICATION SKILLS PUT TELEHEALTH USE IN PERIL
5 REASONS YOU NEED TO TEACH COMMUNICATION SKILLS IN YOUR TELEHEALTH LESSONS
The corporate workplace is experiencing some positive benefits to Generation Z’s less formal communication style, according to a writer for Forbes magazine. He said, “We're already seeing Gen Z's impact in the world and the workplace, especially when it comes to communication — and I think it’s great.”
Learn more about ATI’s new telehealth simulation.
He noted how the corporate world is coming to appreciate the casual, “authentic” influence of Gen Z on today’s communication techniques. And while you, too, may enjoy the informal, frank style of chatting with these young people, you may have a different perspective when it comes to educating students about talking to clients. This is particularly true considering the growing use of telehealth.
Many younger students feel comfortable chatting via video because it’s such a common experience; they’ve had such conversations most of their lives. And, during the pandemic, these conversations have become even more commonplace.
But the flip side to this familiarity is the likelihood of bringing the same casual tone to their professional conversations with clients — particularly when using telehealth options.
That makes students’ need for learning professional communication skills ever more critical, because telehealth is becoming a routine part of healthcare.
 Nicole Corso, MSN, BSN, ATI Nursing Education Specialist, says professionalism is only 1 aspect of providing quality care with this technology.
Nicole Corso, MSN, BSN, ATI Nursing Education Specialist, says professionalism is only 1 aspect of providing quality care with this technology.
“Students not only need to understand how to approach clients compassionately — but not too informally,” she explained, “but they also need to know the best practices for using telehealth. And they need to learn effective techniques for questioning clients about their medical conditions.”
Simulation solutions are an effective option for giving students practice in learning these skills. ATI recently introduced a new screen-based simulation module to its Nurse’s Touch, The Communicator, solution for that purpose. The module, “Client care through telehealth,” is designed to teach both professionalism, best practices, and 1 other crucial skill: motivational interviewing.
This third aspect, Corso said, is especially important for ensuring students become competent, practice-ready nurses.
“When they graduate and move on to their new careers, their employers expect them to be ready on Day 1,” she explained. “Simulation allows them to practice until they feel confident in using telehealth technology so they can hit the ground running.
ELIMINATING THE MYSTERIES OF MOTIVATIONAL INTERVIEWING
"Motivational interviewing isn’t new. It’s been around since 1983, when it was first described in an article published in Behavioural Psychotherapy. But its use has evolved since its original focus on treating problem drinkers.
Today, healthcare providers use motivational interviewing in the care of clients with both chronic and acute medical conditions. But the need for this client-centered technique has become even more important with the growing use of telehealth. And motivational interviewing is a perfect communication technique to pair with the telehealth conversation format given its ease of use in a virtual setting and its powerful impact on client care.
Most nursing programs have begun adding lessons on telehealth to their curricula. But, as mentioned, hand-in-hand with those lessons needs to be instruction on motivational interviewing.
 The importance of motivational interviewing was emphasized in a webinar on telehealth (available in ATI Academy after login to the ATI website), by Kelley Connor, PhD, RN, CHSE, Director of Simulation-Based Education, Boise State University. She explained that students today are typically very comfortable in learning how to use the technology behind telehealth. But these same students almost universally lack the communication skills to use telehealth effectively.
The importance of motivational interviewing was emphasized in a webinar on telehealth (available in ATI Academy after login to the ATI website), by Kelley Connor, PhD, RN, CHSE, Director of Simulation-Based Education, Boise State University. She explained that students today are typically very comfortable in learning how to use the technology behind telehealth. But these same students almost universally lack the communication skills to use telehealth effectively.
That makes motivational interviewing crucial to their use of telehealth technology.
MOTIVATIONAL INTERVIEWING IN REAL-WORLD SETTINGS
The state of Idaho is fairly rural, said Lynda Peel, MSN, RN-BC, CCRNE, Program Manager of Data and Process at St. Luke’s Health Systems (Boise, Idaho) — who also spoke during the telehealth webinar. To help fill in healthcare gaps across the southwest part of the state, Peel said her hospital system began branching out to organizations that didn’t have adequate intensive care support.
 Because her system had a pool of intensive care physicians and nurses, the organization created a virtual hospital setting. In it, virtual nurses offered support in units from med-surg to — when the pandemic hit — COVID units.
Because her system had a pool of intensive care physicians and nurses, the organization created a virtual hospital setting. In it, virtual nurses offered support in units from med-surg to — when the pandemic hit — COVID units.
The nurses working in virtual roles were helping with many tasks, such as dual-signing medications, patient teaching, discharge teaching, admissions, and skin assessments.
The work eventually expanded into RPM, remote patient management. Peel said the hospital system started by working with chronic conditions, such as heart failure, diabetes, and high blood pressure. Recently, it rolled out the treatment of sepsis in COVID-19 patients.
“Patients are becoming more acute,” she added. “It’s no longer a patient who’s had a chronic condition for 3 months before they can qualify for [using RPM]. They’re actually receiving an iPad on discharge and having an RPM nurse talk to them [in the home setting].”
 With this change, motivational interviewing has become “huge,” she said. “We are training all of our remote patient-management nurses in motivational interviewing to help the patient become more involved in their care.” The technique allows St. Luke’s nurses to help clients identify goals and needs, “instead of us telling them what they are going to do to get better,” Peel added.
With this change, motivational interviewing has become “huge,” she said. “We are training all of our remote patient-management nurses in motivational interviewing to help the patient become more involved in their care.” The technique allows St. Luke’s nurses to help clients identify goals and needs, “instead of us telling them what they are going to do to get better,” Peel added.
RESEARCH SUPPORTS THE IMPORTANCE OF MOTIVATIONAL INTERVIEWING
Teaching your students how to perform motivational interviewing will not just help with future telehealth interactions but with client care in general. In fact, research proves the positive impact that this directive, client-centered approach has elicited in behavior change.
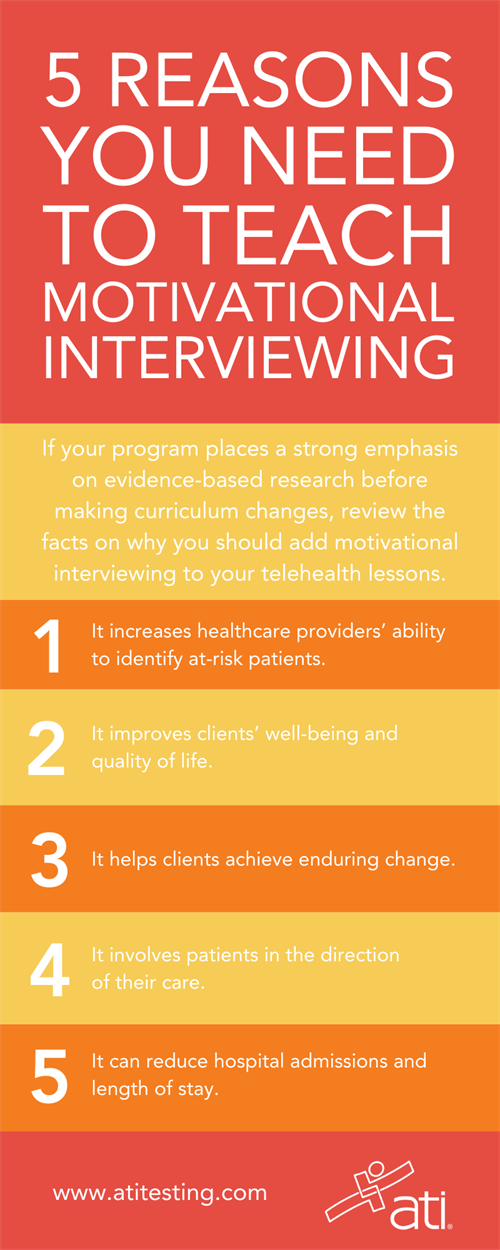
If your program places a strong emphasis on evidence-based information before deciding to make curriculum changes, we’ve gathered some research that may inspire you to incorporate motivational interviewing into your curriculum alongside your lessons on telehealth.
1. MOTIVATIONAL INTERVIEWING INCREASES HEALTHCARE PROVIDERS’ ABILITY TO IDENTIFY AT-RISK PATIENTS.
Consider a study of primary care professionals who participated in simulation training on how to use MI for screening, brief interventions, and referral to treatment with patients suffering from substance use, depression, anxiety, and PTSD. Their goal? To build patients’ motivation and increase protective — AKA healthy — behaviors. In a 3-month follow-up after the study, participants self-reported that they had experienced a 51% increase in identifying at-risk patients.1
 The benefits of this new knowledge didn’t end there. Participants also reported:
The benefits of this new knowledge didn’t end there. Participants also reported:
- 60% increase in patients screened
- 58% increase in patients with whom treatment options were discussed
- 53% increase in collaborative decision-making with patients about treatment plans.
2. MOTIVATIONAL INTERVIEWING IMPROVES CLIENTS’ WELL-BEING AND QUALITY OF LIFE.
Wound-care specialists in the United Kingdom knew that well-being and quality of life were important factors in treating patients with chronic injuries. “Encouraging patients to take medications, engage in healthy lifestyles, and quit harmful habits is vital,” staff wrote in a paper, “Improving well-being and quality of life using motivational interviewing.”2 So they decided to test the theory that MI could positively effect change in their clients.
The results from questionnaires completed by clients before and after attending baseline and follow-up sessions indicated that adding MI to standard care “significantly improved participants’ well-being.” The researchers noted that that it was “important to ask the [client] what optimal well-being is for him or her.”
DOWNLOAD THE INFOGRAPHIC AT RIGHT AS A HANDY REFERENCE
3. MOTIVATIONAL INTERVIEWING HELPS CLIENTS ACHIEVE ENDURING CHANGE.
Nutritionists regularly use MI in helping clients change their eating and activity patterns. In an article in Today’s Dietitian touting the benefits of MI, author Dawn Clifford, PhD, RD, wrote, “Motivational interviewing (MI) is an ideal counseling style for assisting the most ambivalent clients.”3
She continued, “When clients voice personal internal motivations, they are more likely to move toward change than when they are given lists of reasons they should change.”
Similarly, in the paper “The spirit and intent of motivational interviewing,” authors stated that “the concepts and methods of MI are scientifically proven to be effective for developing therapeutic rapport and to enhance positive health behavior changes or recovery during hospitalization.”
They noted that the positive effects were noticeable during observations conducted by psychiatric healthcare providers who could “see the patient’s response being more open to discussion.”5
4. MOTIVATIONAL INTERVIEWING INVOLVES PATIENTS IN THE DIRECTION OF THEIR CARE.
 Smoking cessation is a specific area that has seen positive results from MI. In an interview, Jayne Josephsen, EdD, RN, CCCTM, CHSE, CHPN, professor of nursing at Boise State University in Idaho, said, “What really happens in [the MI] process is that people kind of identify what their values are. They discover that they really want to stop smoking. They want to spend more time with their grandchildren and the rest of their family. Sometimes with small children, people don’t want to smoke around them.”4
Smoking cessation is a specific area that has seen positive results from MI. In an interview, Jayne Josephsen, EdD, RN, CCCTM, CHSE, CHPN, professor of nursing at Boise State University in Idaho, said, “What really happens in [the MI] process is that people kind of identify what their values are. They discover that they really want to stop smoking. They want to spend more time with their grandchildren and the rest of their family. Sometimes with small children, people don’t want to smoke around them.”4
Such realizations, she added, help patients identify what’s most important regarding their overall health and quality of life. This realization gets them more involved in the direction of their care.
5. MOTIVATIONAL INTERVIEWING CAN REDUCE HOSPITAL ADMISSIONS AND LENGTH OF STAY.
A community mental health team (CMHT) in Singapore wondered if their efforts could be more effective if they used MI with their clients. Using a quasi-experimental method, they selected a convenience sample of 120 participants and performed MI with each persona once a month for 1 year. The results? Positive.
“Participants who underwent the CMHT services with MI were more compliant to treatment, resulting in significant reduction in hospitalization and improvement in functionality,” the study’s authors wrote.5
In addition, the researchers determined that MI is effective in facilitating better illness management for patients in the community. “Adoption of the MI approach may potentially provide significant benefits for psychiatric support services in the community,” the authors wrote.
RESOURCES
1Albright G, Adam C, Serri D, Bleeker S, Goldman R. Harnessing the power of conversations with virtual humans to change health behaviors. 2016;2:44. Published 2016 Nov 28. Accessed Jan. 19, 2022.
2Lindsay E, Mechen C. Improving well-being and quality of life using motivational interviewing. Wounds UK. 2018;14(5):138-141. Accessed Jan. 19, 2022.
3Clifford D. Motivational interviewing. Today's Dietitian. 2016;18(7):48-55. Accessed Jan. 19, 2022..
4AHC Media. Motivational interviewing gains strength in patient-centered care. Hospital Case Management. 2018;26(12):153-164. Accessed Jan. 19, 2022.00. Accessed Jan. 19, 2022.
5Mallisham SL, Sherrod B. The spirit and intent of motivational interviewing. Perspectives in Psychiatric Care. 2017;53(4):226-233. Accessed Jan. 19, 2022.
6Chay Huang Tan S, Wen Hui Lee M, Gentatsu Tan Xiong Lim, Jern-Yi Leong J, Cheng Lee. Motivational interviewing approach used by a community mental health team. Journal of Psychosocial Nursing & Mental Health Services. 2015;53(12):28-37. Accessed Jan. 19, 2022.